Program Overview

With a strong track record of post-fellowship career placement and faculty development, the Genitourinary Reconstructive Surgery team at University of Washington seeks to train academic leaders in reconstructive urology. Since its inception in 2005, the fellowship program at UW has continued to innovate and evolve in response to the needs of patients and learners, and to contribute to advancing the field. Building on a foundational understanding of injury mechanisms, ranging from acute trauma to the delayed effects of ionizing radiation and surgery, the program retains an interest in urethral and genital reconstruction while incorporating significant experiences in upper and lower urinary tract abdominal reconstruction and genital gender affirming surgery. UW’s GURS program is recognized as the pre-eminent institution in the Pacific Northwest for robotic and open abdominal urologic reconstruction, with patients traveling from across the WWAMI region and other parts of the nation to pursue reconstructive ureteral and bladder surgeries with our team. In addition, UW Medicine’s Genital Gender Affirming Surgery program draws from a national referral base to meet the primary and revision surgical needs for a large number of transgender and gender diverse patients.
Graduates
The Fellow works closely with UW School of Medicine faculty including Program Director Hunter Wessells, Judith Hagedorn, Alexander Skokan, and Army urologist Jonathan Wingate. In addition to extensive experience with open and endoscopic treatment of urethral pathology and comprehensive genital reconstruction, the fellow will gain significant experience with robotic reconstructive surgery utilizing both the DV5 multiport and SP single port platforms, including critical assessment of the role for each platform in independent practice. The fellow benefits from extensive collaboration with faculty in Orthopaedic, Colorectal, Plastic, and Trauma General Surgery to develop shared mental models and multidisciplinary surgical planning for the most challenging cases. The surgical management of complex male urinary incontinence, salvage placement of erectile implants, surgical treatment of Peyronie’s Disease, and repair of complex pelvic fistulas round out the clinical training experience.
Program Graduates, 2005-present
The Fellow is expected to supervise a limited independent clinic (2 days/month, 10% time), has 1 day/week of dedicated time for research and education (20% time), and otherwise participates in operative and ambulatory patient care with the GURS faculty through a structured clinical experience with an emphasis on graduated autonomy (70% time). Trauma call has long been a feature of the fellowship, with the fellow supervising residents for urologic trauma cases when on call, and in turn backed up directly by a GURS faculty with significant urotrauma experience; there is no expectation for participation in the general call pool or staffing of non-traumatic on call consults/cases.
A robust educational program includes weekly Reconstructive Urology teaching conferences, periodic journal clubs, and recurring lectures from a host of faculty from collaborating specialties. The Fellow’s clinical experience includes daily partnership, supervision, and education of urology residents, advanced practice providers, and rotating medical students. The Fellow works with the GURS faculty to coordinate a monthly genitourinary trauma & reconstructive research work group, a productive venue for the development, execution, and dissemination of clinical research projects in the field.
Graduates have advanced in academic departments, cancer centers, and community practice. Significant contributions to the field of GU trauma and reconstruction include their participation in AUA and ACS Guidelines, the TURNS Network, the AUA Core Curriculum, as well as through NIH funded grants and leadership of centers of excellence in gender affirming surgery and new fellowship programs.
Program Leadership

Hunter Wessells, MD, FACS
Program Director
Length of Fellowship
One year
Number of fellowships available
One position per year
Faculty
Since inception of this fellowship in 2005, the participating faculty has grown from one fellowship-trained reconstructive surgeon to four. Hunter Wessells, MD, FACS initiated the fellowship in 2005. Judith Hagedorn, MD, MHS, FACS, joined in 2016 and Alexander Skokan, MD and Jonathan Wingate, MD joined in 2020.
Current fellow
Ryan Haggart, MD
Goals and Objectives
The goal of advanced training in trauma and reconstructive urology is to impart further knowledge and skills beyond the expertise achieved during a urology residency program. The additional expertise should include critical analysis of complex clinical problems, development of advanced technical skills, and scholarship. The fellow should further enhance his/her skills in the planning of multidisciplinary approaches to patient care and mature his/her knowledge in clinical research methodologies.
After completing a one-year minimum fellowship in trauma and reconstructive urology, the graduate should demonstrate the following unique characteristics:
- Ability to perform complex urethral and genital surgery with a clear understanding of the benefits and the technical limitations of surgical procedures
- Advanced expertise in the multidisciplinary management of patients with urologic trauma
- Knowledge and the ability to apply the critical principles of plastic surgery and urology imaging techniques
- Extensive knowledge of and technical experience in lower urinary tract reconstruction and male incontinence surgery (AUS, male urethral sling)
- Significant knowledge of and technical experience in abdominal urinary tract reconstruction, including selection of appropriate use cases for multi-port robotic, single port robotic, endoscopic, and open approaches to surgery
- Significant experience with decision-making and technical components of genital gender affirming surgery, including primary and revision surgeries
- Knowledge of the biology of injury and wound healing
- Comprehension of and facility with scientific methodology, study design, biostatistics, and data analysis
- Ability to manage academic or tertiary referral clinical practice and participate in continuing education
- Skills for self-education and collaboration in translational research
Research Opportunities
The University of Washington is one of the top research institutions in the United States.
Research is encouraged under the supervision of an appropriate mentor. There are many opportunities for the fellow, and we fully support exploring new avenues for research based on the fellow’s desires/goals. Approximately 20% effort is allocated for research. The Harborview Injury Prevention and Research Center (HIPRC) allows fellows to participate in one of the leading institutions researching how and why people suffer injuries. There are many available databases for research projects – Harborview Medical Center Trauma Registry, National Trauma Data Bank, Crash Injury Research Engineering Network, Washington State Comprehensive Hospital Abstract Reporting System (CHARS), among others. The prospective fellow will be an integral part of the monthly research meetings which are attended by faculty, residents and medical students involved in reconstructive/trauma research projects.
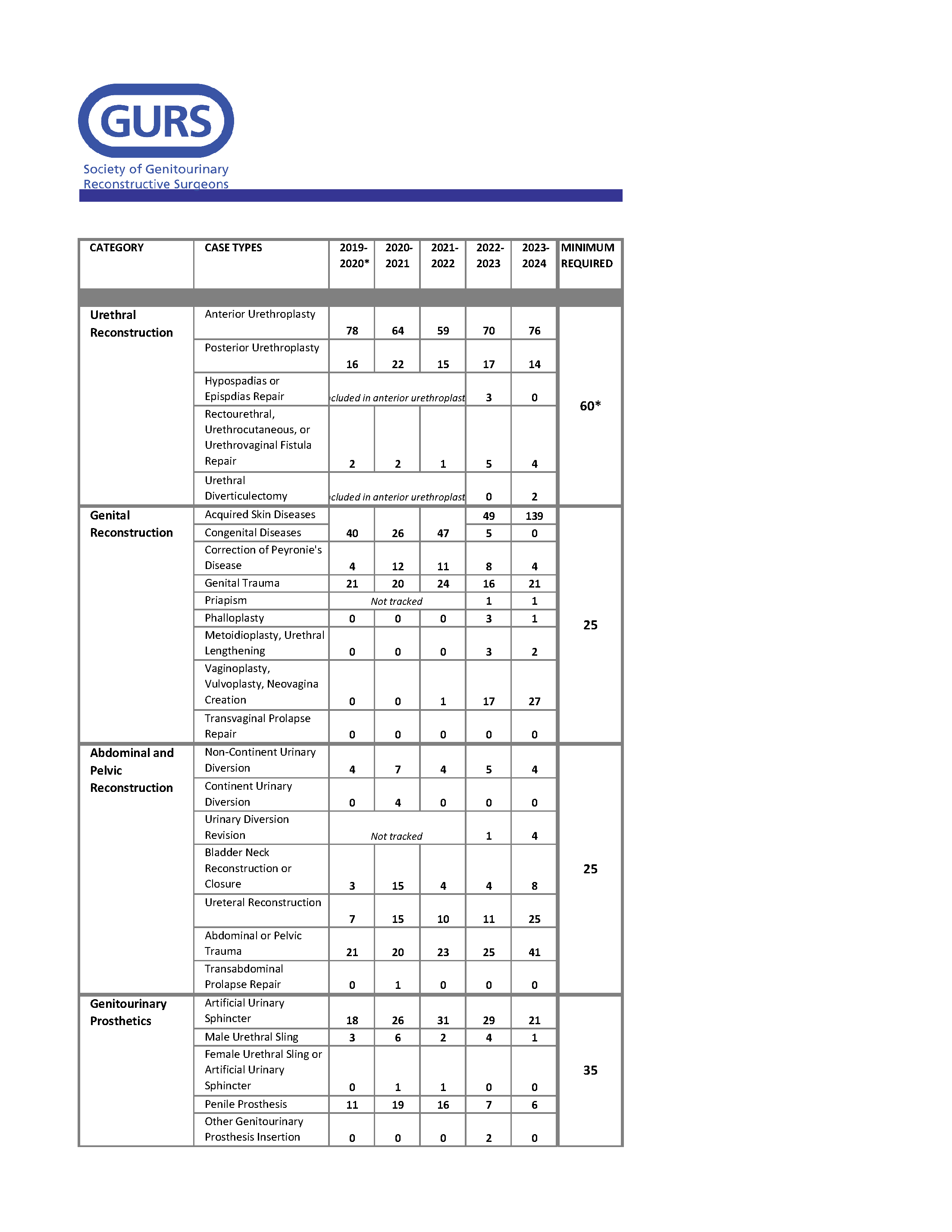
Surgical Case Log
Application Requirements
Candidates must have completed an ACGME-approved residency in urology or the equivalent. The applicant must have passed all 3 steps of USMLE exam and be eligible for a WA State Medical License.
- Admission is contingent upon completion of an ACGME accredited urologic training program or an appropriate foreign program.
- Applicants must be eligible for or possess a Washington State Medical License.
- In order to be eligible for University sponsorship for an H-1B visa, graduates of foreign (non-U.S.) medical schools must show successful completion of all three steps of the U.S. Medical Licensing Exam (USMLE), or equivalent as determined by the Secretary of Health and Human Services.
Application materials
- GURS Application Form
- Curriculum Vitae
- Personal Statement
- At least 3 letters of recommendation, including at least one letter from their urology training program director and/or department chair recommending them for the fellowship and attesting to the candidate’s successful completion of the urology training program.
Application deadline: Sunday, January 4, 2026 at 11:59pm ET
All applications will be reviewed after the deadline and interview offers made following review of all completed applications submitted by the deadline.
Interview Format: virtual interviews
Interview dates: Wednesday, March 18, 2026
Match date: June 29, 2026
All applications will be processed through the official UW Supported Hiring Portal, Interfolio to be considered.
University of Washington Hiring Policies
The University of Washington is committed to fostering an inclusive, respectful and welcoming community for all. As an equal opportunity employer, the University considers applicants for employment without regard to race, color, creed, religion, national origin, citizenship, sex, pregnancy, age, marital status, sexual orientation, gender identity or expression, genetic information, disability, or veteran status consistent with UW Executive Order No. 81.
For More Information
Virtual Open House: Wednesday, December 17, 2025 from 5-6pm PST
University of Washington Department of Urology
Box 356510
1959 NE Pacific St., BB-1114
Seattle, WA 98195-6510
Phone: 206-221-1509
Fax: 206-543-3272
urofellow@uw.edu