UW Medicine Department of Urology in the COVID-19 Pandemic
The COVID-19 pandemic placed unprecedented strain on health care systems throughout the world, balancing appropriate and necessary health care with measures to minimize virus transmission. As the leading academic medical center in one of the first US cities to be hit, UW Medicine Urology has been involved in surgical triage, redeployment plans, telemedicine implementation, as well as a project to predict the long range impact of care deferral on the urological health of our population.
Immediate Responses Of Urology Departments
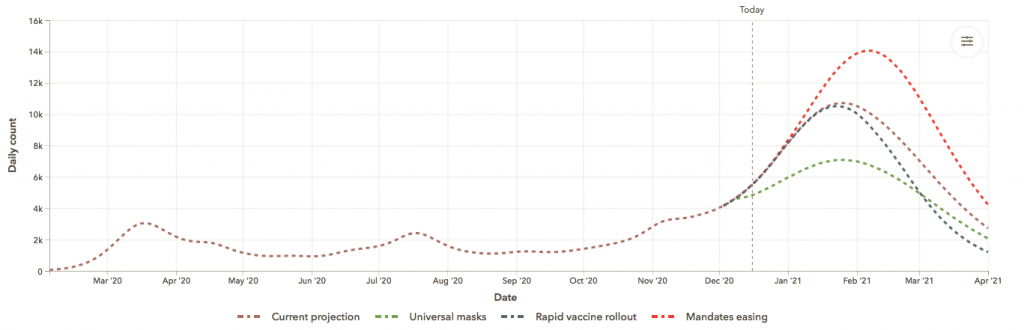
Faced with a rapid upswing in COVID-19 cases during the month of March 2020 (see Figure 1 for Washington State), the Department took measures across UW Medicine, Seattle Childrens, and the Puget Sound VA to address resource constraints, restrictions on elective surgical cases, and protection of our workforce. Each hospital made day-to-day changes in response to supplies of personal protective equipment (PPE) and front line staffing needsd. Although few members of the Department ultimately were called to serve, an overwhelming number of residents, fellows, advance practice providers and attending urologists volunteered to do so, demonstrating our collective duty of caring.
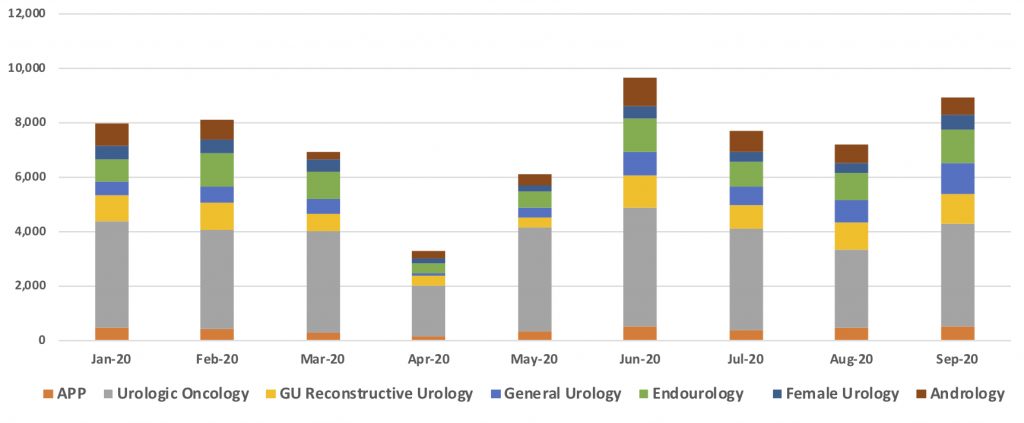
Surgical services across Washington rapidly ceased elective surgery in response to state Executive Orders. The American College of Surgeons on March 17th issued triage guidance for non-emergent surgical care (American College of Surgeons, 2020). The unsurpassed testing capacity for coronavirus by UW Medicine laboratories allowed universal testing of surgical patients to be implemented almost as soon as the pandemic hit. To provide emergency surgery for trauma, necrotizing soft tissue infection, and urinary obstruction, the Department deployed platoons of on-call teams. Elective urological surgery was canceled, with the exception of selected patients with active urinary stone disease (Metzler et al, 2020) and those with high risk malignancies (e.g. aggressive bladder, kidney and other cancers). The variation in care delivered by each urological subspecialty reflected hospital policies and access to PPE (see Figure 2). As we now sit in the midst of a second major surge in COVID-19 cases across the state, UW Medicine has implemented a revised triage approach suspending only elective and low acuity surgery that requires allocation of a hospital bed. In comparision to the first wave in March, the November surge is having the biggest impact on nursing staff and inpatient and ICU bed availability. The surgical volume reduction is designed primarily to preserve inpatient capacity for projected larger number of hospital admissions across UW Medicine.
Telemedicine
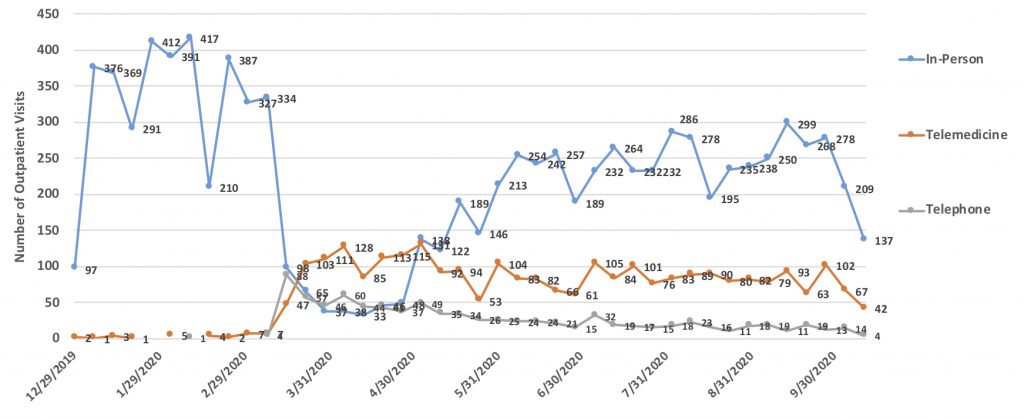
Telemedicine evolved as an important means to sustain essential patient care during the pandemic, with additional benefits of protecting patients and healthcare providers from potential exposure. The rapid adoption by our Department will permanently change care delivery and accelerate the digitalization of healthcare. The trends in outpatient encounters (see Figure 3) for the Department at UW Medicine show near complete cessation of in person office visits in March and April of 2020. A commensurate rise in telemedicine and telephone visits allowed 50% of outpatient visits to continue. Converting in-person visits to telemedicine will continue to be key to managing successive waves of COVID-19 infection; rising rates of community transmission will affect members of the healtcare team and require management of workplace and household exposure to the coronavirus.
Long term Consequences Of Covid-19 On Urological Care
Deferred care as a result of COVID-19 will impact every specialty of medicine and surgery, and these may be far reaching. Delays in care for urologic emergencies such as urinary obstruction, hematuria, nephrolithiasis, and urologic trauma can have severe sequelae. It is evident that the COVID-19 pandemic has contributed to significant variation in the presentation of emergent urologic conditions, although the short and long-term implications remain to be investigated.
The pandemic also has uncovered disparities in impact of the disease by race, ethnicity, and other factors (Price-Heywood et al, 2020).
A team of UW Urology researchers assembled to study emergency access and overall urological healthcare visits during the period before and during the COVID-19 pandemic. Rishi Sekar MD, a rising Chief Resident, and Sarah Holt Phd, members of the Urology Research and Outcomes Collaborative, analyzed the reduction in frequency of urologic care-seeking early in the pandemic and burden of unmet urological conditions. Notably, the concurrent increase in telemedicine use during the pandemic also may create health disparities related to access to technology. Future analyses will focus on detailed trends with care access and utilization by demographic groups and urologic subspeciality.
Conclusions
The COVID-19 pandemic affected every aspect of healthcare and will have a lasting impact on many facets of urological patient care. The reduction in access to outpatient consultation and elective surgery will translate into more complex management due to deferred care; delays in cancer screening; a reduction in routine and emergency diagnostic studies that detect serious urological conditions; lower case numbers for trainees; and challenges for clinical trials and basic research. The collaboration and innovation required to meet patient needs and protect healthcare workers will yield important advances including digitalization of the outpatient and inpatient envirnoments, remote care delivery and new clinical trials approaches. UW Urology will be conducting further research to identify vulnerable populations that may have experienced greater impact from COVID-19 illness, limted access to telemedicine, and a larger burden of deferred care of non-emergent urological conditions.
FIGURE LEGENDS
- Covid-19 case rates in Washington State, March-November (Instittue for Health Metrics and Evaluation, accessioned November 22, 2020 at https://covid19.healthdata.org/united-states-of-america/washington?view…
- Clinical activity including outpatient and surgical cases as measured by work relative value units (wRVU) and subspecialty within UW Medicine Department of Urology. Note the total reduction in volumes (Y axis, wRVU) by month with a nadir in April 2020, rebound in June 2020 reflecting backlog of untreated surgical cases, and return to baseline levels of clinical activity. All subspecialties experienced reduced volumes, with degree of reduction and time to recovery varying substantially. APP: advanced practice provider.
- Outpatient visit volumes by type within UW Medicine Department of Urology. Note previous nominal use of telehealth prior to March 2020.